“Whole-person care is critical for improving health outcomes because human wellness depends on multi-dimensional, multisystemic care coordination. People’s social, emotional, economic, and environmental conditions affect their health.”
April 7th is World Health Day! To celebrate, we’re talking about whole-person care and its benefits, as well as the Power Threat Meaning framework that has been developed abroad. As champions for improved access to resources for those living with behavioral health conditions, we know that our current healthcare infrastructure could benefit from a reimagining. We firmly believe that mental healthcare is healthcare. We believe that incorporating behavioral and mental healthcare into primary care settings can help reduce the stigma surrounding these conditions. And most of all, we believe that healthcare should treat patients and people as entire, holistic beings.
What is Whole-Person Care?
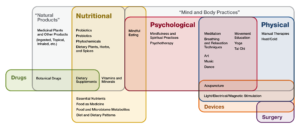
Whole-person care “is the patient-centered optimal use of diverse healthcare resources to deliver the physical, behavioral, emotional, and social services required to improve care coordination, well-being, and health outcomes while respecting patients’ treatment choices.” Basically: whole-person care is about treating every part of an individual, through every avenue available. By using diverse resources and therapies, an individual seeking care is more likely to feel supported physically, emotionally, mentally, and spiritually. Whole-person care is all about the patient: finding care that works and coordinates well with other treatments to create a holistic approach to healthcare.
Though integrative and whole-person medicine has existed for centuries, it made its first popular appearance in modern medicine in the 1970s. Since then, whole-person care has been integrated into multiple states’ approaches to healthcare: from extensive studies to pilot programs, healthcare has experienced a renaissance of integrative medicine. Whole-person, integrative, and patient-centered care take into account the additional issues that impact individuals’ health beyond simply the physical: chronic stress, socio-economic determinants of health, and mental and behavioral health concerns.
This kind of care goes beyond treating the symptoms of an illness or ailment: rather, whole-person and integrative care systems consider alternative therapies in addition to traditional medicine. Noetic therapies, nutrition, yoga, mindfulness, hypnosis, acupuncture, and aromatherapy all count in whole-person, integrative care. Alternative activities are not preferred or pursued in place of traditional medicine: instead, they are combined to create a multi-disciplinary approach to care that addresses many aspects of a person’s health. Traditional medicine remains a vital and important part of the equation, but it doesn’t have to be the entire equation. Whole-person care expands the traditional medical setting to incorporate multidimensional approaches: a patient’s emotional, mental, and spiritual wellbeing become as important as physical health in a whole-person care setting.
What are the Benefits?
Our bodies are made up of many interconnecting systems: everything is connected to something else, and these connections and intersections impact our overall health. Treating just one aspect of the whole is often not enough.
Behavioral and mental health are often overlooked when it comes to healthcare: these aspects of our health are considered more difficult to treat, and therefore fall by the wayside in traditional medical models. In a whole-person care setting, the treatment is patient-centered and driven. This means that any concern a patient has is relevant, important, and will be taken into account when considering treatment options.
Whole-person healthcare allows providers and patients to create personalized health plans. It also allows providers to be more conservative with prescriptions. Over-prescribing medication to treat a patient can lead to more behavioral health issues and open the door to dependency. Of course, medication can be a lifesaver – the key is to know when it is necessary. With whole-person care, treatment plans don’t have to revolve around medication: rather, it can be one aspect of a larger and more connected approach.
Not only does whole-person care provide more options, but it also creates a culture of collaborativity between providers. Patient-centered, whole-person care can lower operating costs for hospitals and care facilities, lead to faster recovery times, increase overall satisfaction, and improve the quality of patients’ health.
Medical conditions and behavioral health conditions go hand in hand. When an adult faces serious mental health concerns, it is far more likely that they will develop a general health condition as well. This is called comorbidity: the presence of two or more health conditions that interact and compound to create worse health outcomes. Comorbidity has been shown to adversely affect people in significant ways: often, one health issue hides behind another, and vice versa. One of the best ways to tackle comorbidity involves finding complementary ways to address an individual’s health.
The Power Threat Meaning Framework
In the UK and other countries abroad, a framework has emerged that allows us to see behavioral and whole-person health in a new light. The Power Threat Meaning Framework considers socio-economic factors, lived experience of trauma, and personal coping mechanisms. The three pillars of this framework are power, threat, and meaning: how power has impacted your life, how misuses of power have led you to develop threat responses, and how you have made meaning out of those responses. These threat responses are our behaviors, symptoms, and internal experiences. Nothing happens in a vacuum: we are all impacted by power structures, and misuse of power often results in difficult and adverse experiences, which can be known as trauma. The PTM framework was developed by a team of service providers and service users (in other words, people with lived experience of large-scale distress). However, this framework can be helpful to all of us.
The goal of the PTM framework is to allow people to create more hopeful and constructive narratives about their experiences. Rather than label ourselves as “mentally ill,” the PTM framework allows us to see the wider social structures that have impacted our lives. Our symptoms and experiences of behavioral health conditions can be seen as the ways in which we have survived and resisted the misuse of power in our lives.
The framework “highlights the links between wider social factors such as poverty, discrimination and inequality, along with traumas such as abuse and violence, and the resulting emotional distress or troubled behaviour.” This framework is not meant to replace any existing models of healthcare; instead, it offers a new way to look at our experiences. It simply provides a new lens through which to view our lives. Pattern recognition is vital in the PTM framework: we all develop patterned responses to threats in our lives, and these patterns become normal for us.
These questions can help you use the framework to address your own experiences in a new way:
- What has happened to you? (How is Power operating in your life?)
- How did it affect you? (What kind of Threats does this pose?)
- What sense did you make of it? (What is the Meaning of these situations and experiences to you?)
- What did you have to do to survive? (What kinds of Threat Response are you using?)
The PTM framework states that we are all working to live and exist in an imperfect society. There are so many factors that might impact our health that are beyond our control. This lens allows us to reimagine our experiences as ways of survival, not just symptoms. We make meaning out of our experiences – we reinforce patterns over time. The PTM framework allows us to examine those patterns as they exist in their relationships with wider social factors.
Reimagining Care in Colorado
You can start using the whole-person care model in your own life, right now, as well as the Power Threat Meaning framework. We encourage you to see your health as a big picture, rather than just a piece of the puzzle. We are intimately influenced by social, economic, and structural power – our experiences are reflections of the world that we live in. This month, reimagine your own healthcare as something holistic and connected. Approach your health knowing that you are a whole being, a person with many facets. The next time you visit your primary care physician, keep in mind that we cannot dissect ourselves into parts: we exist as a whole. When it comes to mental and behavioral health, acknowledge the ways in which power has influenced your life. Examine your patterns: your responses to threat and the meaning you have made out of those threats. We don’t have to wait for our healthcare system to catch up in order to care for ourselves wholly. We can and must see ourselves as connected, whole people.